Orthopedic Medical Billing Guide: Challenges and Strategies for RCM Teams
Discover how medical billing for orthopedic practices works, the key challenges involved, and strategies RCM teams can use to reduce denials and boost revenue.
October 4, 2025


Key Takeaways:
• Orthopedic billing is complex due to multi-step procedures, implants, and lengthy global periods. Frequent CPT, ICD-10, and payer rule changes make compliance a moving target.
• Most denials stem from documentation gaps, modifier misuse, and missing prior authorizations.
• Accurate coding, real-time eligibility checks, and proactive denial tracking are key to faster reimbursements.
• AI-powered orthopedic medical billing software can help automate coding, scrubbing, and claim follow-up.
Most revenue cycle teams know orthopedic medical billing is complex. Surgeries often involve multiple procedures, devices, and long recovery windows that stretch across global periods.
But the way RCM teams work is shifting. Fast.
New CPT and ICD-10 updates are released each year, payers apply their own ever-changing rules, and prior authorizations add another layer of delay. Billing teams are expected to juggle documentation, coding, claim edits, and appeals—all while keeping up with compliance standards that move faster than most workflows can handle.
Add to that the rise of high-cost implants and payer scrutiny on modifiers, and orthopedic billing requires more than just “getting the codes right.” It demands new strategies, smarter tools, and a more proactive approach to managing the revenue cycle.
This guide explores the biggest challenges in orthopedic medical billing today and the strategies RCM teams can use to stay compliant, reduce denials, and protect revenue.
What Is Orthopedic Medical Billing?
Orthopedic medical billing is the process of converting the specialized care orthopedic providers deliver into the standardized codes and claims insurers require for reimbursement. It bridges clinical documentation and financial accuracy, ensuring that every procedure, device, and follow-up visit is properly recorded, coded, and paid for.
An Overview of the Orthopedic RCM Workflow
The orthopedic revenue cycle management (RCM) workflow involves the following steps:
- Patient Registration & Insurance Verification: Eligibility checks confirm that coverage is active and that orthopedic services, such as imaging or surgery, are included in the patient’s plan.
- ClinicalDocumentation: Providers record the clinical encounter, including exam findings, imaging, surgical details, and any implants used.
- Coding: Coders then assign CPT, ICD-10, and HCPCS codes, adding modifiers when needed. In orthopedics, getting laterality (right vs. left), encounter type, and implant details correct is crucial for clean claims.
- Billing and Claim Submission: Once coded, the visit is converted into a claim. Before it is sent to the payer, billing systems apply edits and scrubbers to catch errors against payer rules and NCCI guidelines.
- Denial Management and payment posting: After payers process the claim, payments are posted to patient accounts. Any denials are reviewed, corrected, and appealed if appropriate.
.webp)
What Makes Orthopedic Medical Billing Hard?
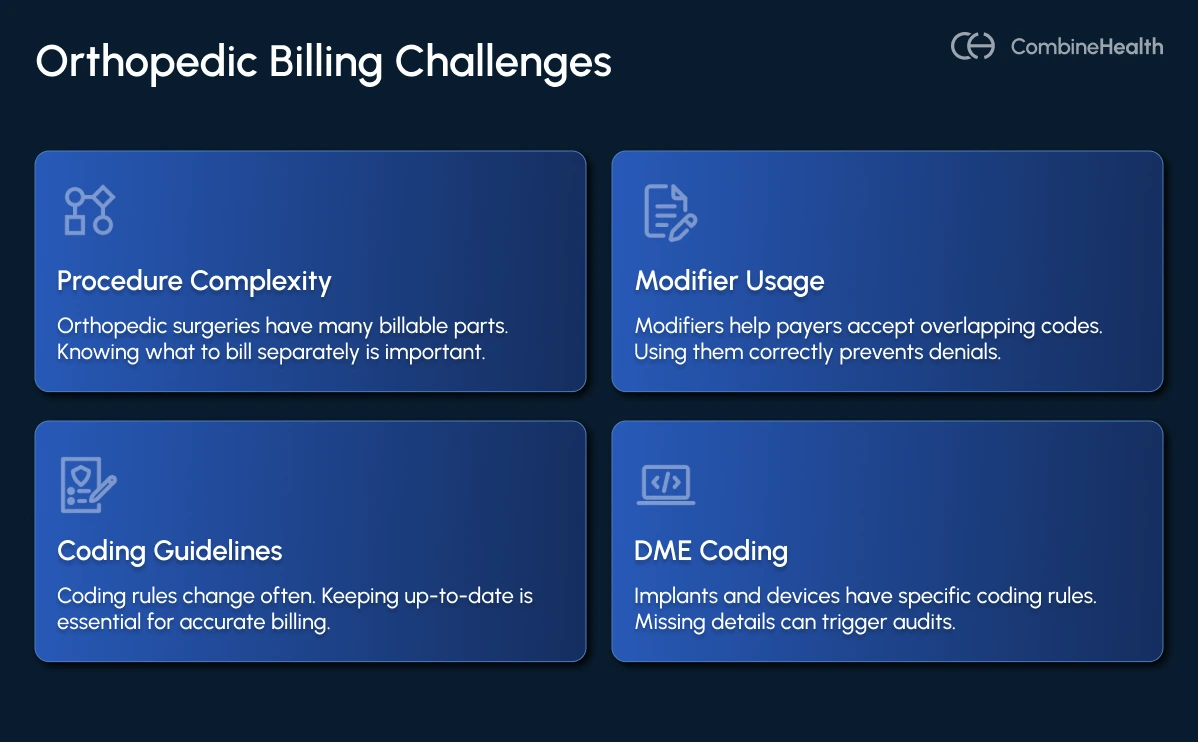
Orthopedic billing is among the most difficult specialties because it blends high-cost procedures with some of the most detailed coding rules in healthcare. Here are the most common factors that make billing for orthopedics so challenging:
- Procedure complexity and multiple components: Orthopedic surgeries often contain multiple billable elements, including the surgical approach, repair vs. reconstruction, grafts, implants, and ancillary procedures such as arthroscopy or debridement. Identifying which actions are separately billable versus bundled into a surgical package is critical to avoid underpayment or denial.
- Modifier usage and specificity: Modifiers determine whether payers accept overlapping codes. Misuse or omission of modifiers is a leading cause of claim denials and payer audits.
- Stringent coding guidelines and diagnosis specificity: CPT, ICD-10, HCPCS, and payer rules are updated annually (sometimes midyear), which makes staying current essential. ICD-10 also requires laterality, encounter type, and high specificity for musculoskeletal conditions; vague diagnoses frequently result in denials.
- DME / implant/ device coding: Implants, prosthetics, braces, and orthoses come with their own coding and documentation rules. Missing implant details, such as model, serial number, or lot, is a common audit trigger.
Orthopedic Billing Guidelines in 2025
New updates in orthopedic coding and billing guidelines introduce changes to coding, bundling, and device documentation that directly impact reimbursement. Here are some updates you should know about:
- ICD-10-CM and ICD-10-PCS Updates: The new CMS guidelines, effective October 1, 2024, expand coding for fractures, musculoskeletal injuries, and orthopedic complications. Practices need to capture laterality, encounter type, and detailed injury descriptions to avoid denials.
- CPT 2025 Code Set: AMA added more than 270 codes, including changes for musculoskeletal procedures. Orthopedic workflows will see updated rules for surgical coding and E/M clarification.
- NCCI Policy Manual 2025: The manual refines bundling/unbundling rules and highlights modifier protocols. Orthopedic billing teams should pay special attention to shoulder and knee surgery edits and correct the use of modifiers 59, XS, LT, and RT.
- LCD & Policy Article Revisions: Medicare contractors introduced new HCPCS codes and coverage criteria for orthopedic supports like ankle-foot and knee orthoses. Documentation must now reflect device specifics to ensure coverage.
Essential Codes for Orthopedic Medical Billing
Orthopedic practices must be fluent in CPT, ICD-10, HCPCS/HCPCS II, and supply/implant codes. Below is a deeper map of what matters and how to organize your coding infrastructure:
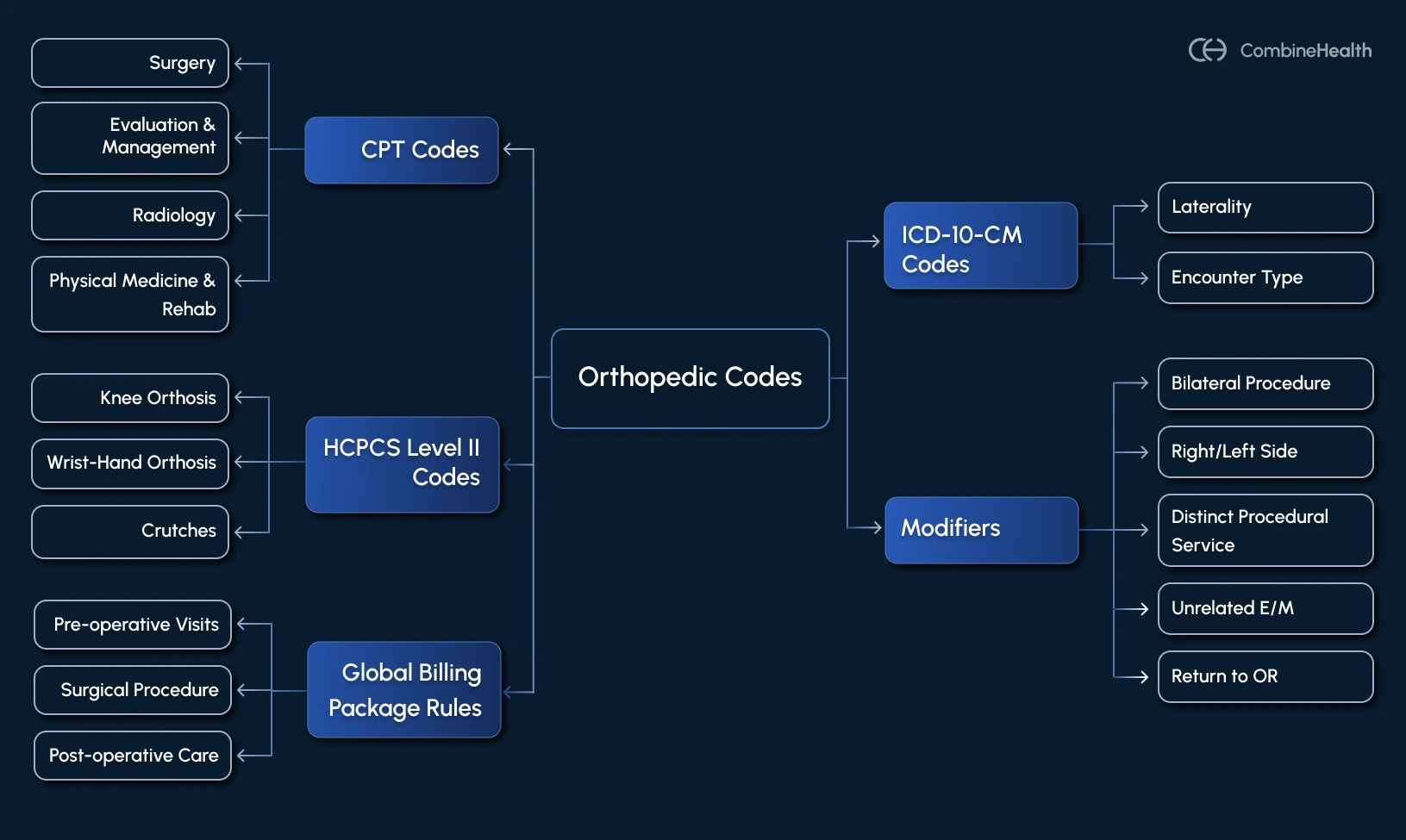
1. CPT Codes: Services and Procedures
Current Procedural Terminology (CPT) codes describe the medical services and procedures provided. In orthopedics, the most commonly used categories include:
- Evaluation & Management (E/M)—99201–99499: These codes cover office visits, consults, and follow-ups. Correct selection depends on history, exam, and medical decision-making. With the 2025 E/M guidelines, documentation must clearly justify complexity, not just time spent.
- Surgery—10021–69990: This is the largest section for orthopedics, covering everything from fracture repairs to joint replacements.
- Radiology—70100–79999: Imaging is central to orthopedic diagnosis and follow-up. Codes in this category apply to X-rays, MRIs, CT scans, and ultrasound guidance for procedures.
- Physical Medicine & Rehab—97000 series: Post-op care often includes therapy services. These codes ensure practices capture revenue for rehabilitation and ongoing musculoskeletal management.
The table below highlights some common CPT codes in orthopedic billing:
2. ICD-10-CM Codes: Diagnosis and Specificity
ICD-10 diagnosis codes explain why the service was performed. In orthopedics, denials often result from vague or incomplete coding. The 2025 ICD-10 updates introduced additional musculoskeletal and fracture-related codes.
Here are some points to consider:
- Laterality is required: Always code whether the condition affects the right, left, or bilateral site.
- Encounter type matters: Initial encounter (A), subsequent encounter (D), or sequela (S) must be noted.
The table below highlights some common ICD-10 codes used when billing for orthopedic:
3. HCPCS Level II Codes: Devices and Implants
Orthopedic billing often involves high-value supplies, implants, and durable medical equipment (DME). HCPCS Level II codes capture these items when they are not bundled into a CPT procedure.
The table below highlights some common orthopedic HCPCS examples:
4. Modifiers
Correct use of modifiers ensures payers process claims accurately. For orthopedics, some of the most important modifiers are highlighted in the table below:
5. Global Billing Package Rules
A global billing package (also called the global surgical package) is the set of rules payers use to decide what’s included in the payment for a surgery and what can be billed separately.
Think of it like a “bundle deal.” When you bill for an orthopedic surgery (say a hip replacement), the payer isn’t just paying for the operation itself—they’re also paying for the standard care that normally comes before and after that surgery.
Medicare (CMS) sets the official framework through the Medicare Physician Fee Schedule and the Medicare Claims Processing Manual.
So, what’s included in the global package:
- Pre-operative visits (after the decision for surgery is made).
- The surgical procedure itself.
- Typical post-op care, such as wound checks and routine follow-up visits, for up to 90 days after major procedures (10 days for minor surgeries).
Not everything is bundled. If care goes beyond what’s normally included, you can (and should) bill it, but only with the right modifier and documentation:
- Modifier 24: Use for an unrelated E/M service during the global period (example: a patient returns with a new hip pain unrelated to their knee replacement).
- Modifier 78: Use when a patient needs to return to the OR during the global period for a complication related to the original surgery.
- Modifier 79: Use for an unrelated procedure or surgery performed during the global period.
Orthopedic Medical Billing Mistakes That Often Cause Denial
Even the most experienced billing teams can slip up when handling orthopedic claims. Understanding the most common mistakes upfront helps orthopedic RCM teams prevent them before claims ever reach the payer.
Mistake 1: Unbundling of Services
Unbundling happens when you bill separate codes for things a payer considers part of a single, inclusive service. In orthopedics, this is a live problem because many surgeries contain multiple steps, supplies, and post-op care that payers treat as packaged into the primary procedure.
When a claim tries to extract one of those pieces, it often trips automatic NCCI or MUE edits and gets denied.
So, how to avoid this?
- Add payer-specific NCCI and MUE rules to your pre-submission scrubber so bundled items are flagged before claims go out.
- Maintain a local “bundle vs separate” rulebook for your top 50 CPTs and push those rules to both clinical staff and coders.
- Train perioperative staff and coders on your bundled scenarios so charge capture is consistent.
Mistake 2: Inappropriate E/M Plus Procedure Billing for Orthopedic
An E/M code plus a procedure code can be billed together when the clinician provides both evaluation or management and a procedure during the same encounter. However, it’s only allowed when the E/M is a distinct and separately identifiable service from the procedure.
Payers deny these claims when the chart does not clearly show two different services happened, or when the documentation does not show separate medical decision making for the E/M.
Let’s clear this up using these examples:
Scenario: New problem -> evaluation + plan, then a procedure
Patient has new right knee instability. You evaluate, decide to order an MRI, and start PT. Later, on the same visit, you aspirate the knee.
Documentation to use: “E/M for new right knee instability—MRI ordered and PT initiated. Therapeutic aspiration performed later; E/M is distinct.”
Scenario: Visit is only for the procedure
Patient comes in for a scheduled knee aspiration. Note documents only the procedure and immediate tolerance.
Documentation to use (if truly separate, it would need more): “Procedure visit only—aspiration performed; no separate E/M.”
Mistake 3: Missing medical necessity, image-guidance proof, or Prior Auth for Injections
Payers commonly deny injection claims when the chart lacks evidence of prior conservative treatment (example: physical therapy), missing proof that image guidance was used when billed, or no prior authorization was obtained. These gaps make the service look nonessential or bundled with another visit.
Mistake 4: Modifier Misuse
Applying a modifier without documentation proving the service was truly separate invites payer denials because it lacks the clinical justification required for separate payment. For example, showing a different anatomic site, a distinct incision, or a separate encounter in the documentation.
Here’s why payers deny it:
Payers and automated edits treat some modifiers as a way to bypass bundling rules. If the chart doesn’t show the clinical fact that justifies the modifier, the claim is flagged and denied.
Key Performance Indicators (KPIs) for Orthopedic RCM
Here are some critical orthopedic RCM metrics to track and benchmarking guidance:
How can AI help with Orthopedic Medical Billing
Traditionally, orthopedic billing teams spend hours cross-checking charts, coding modifiers, and chasing denials. Yet, errors and delays still slip through.
This is where AI can bring an operational advantage by optimizing these RCM processes:
- More accurate coding: AI can scan operative notes and documentation to suggest CPT, ICD-10, and HCPCS codes, along with the appropriate modifiers. This helps reduce errors tied to missed details like laterality or encounter type.
- Smarter pre-submission checks: Instead of waiting for a payer denial, AI scrubbing engines apply payer rules, NCCI edits, and global package policies before the claim leaves your system.
- Handling prior authorizations and eligibility: Because orthopedic procedures often require pre-approval, AI systems can automatically flag when a PA is needed, populate the request with relevant clinical details, and track the status.
- Automating routine claim follow-up: AI can take over repetitive tasks such as checking claim status, posting payments, or drafting appeal letters, freeing staff to focus on complex cases or clinical documentation.
- Transparency and audit readiness: Well-designed AI systems provide an explanation for their coding or billing suggestions. That makes it easier for coders and providers to validate the logic and defend claims in the event of an audit.
- Identifying payer patterns: By analyzing claim history, AI can highlight which payers frequently deny certain procedures, predict which claims are at risk, and suggest adjustments before submission.
.webp)
Transform Orthopedic Billing With Intelligent Automation
Orthopedic medical billing is complex by design, with layered coding rules, global periods, device documentation, and payer edits that rarely stand still.
Looking ahead, the real opportunity is to stop playing catch-up and start building proactive systems that anticipate payer requirements before claims go out the door. With structured processes, up-to-date guidelines, and intelligent automation, orthopedic groups can transform billing from a source of revenue leakage into a steady, reliable part of practice growth.
Ready to see how autonomous AI can support your orthopedic billing team? Book a demo with CombineHealth and explore how our AI workforce helps reduce denials, shorten A/R cycles, and keep revenue predictable.
FAQs
What is medical billing for orthopedics?
Orthopedic medical billing converts clinical care (from evaluations to surgeries) into standardized insurance claims using CPT, ICD-10, and HCPCS codes. It ensures providers are reimbursed accurately for musculoskeletal treatments, implants, and post-operative care.
Is orthopedic billing hard?
Yes. Orthopedic billing is complex because it involves multiple procedures, detailed documentation, strict modifier rules, global periods, and frequent payer-specific updates.
What are the orthopedic medical billing requirements?
Accurate documentation, correct CPT/ICD-10 coding, proper modifier use, compliance with global package rules, and payer-specific prior authorizations are essential to avoid denials and ensure timely reimbursement.
What is the CPT code for orthopedic services?
Orthopedic services use CPT ranges for E/M (99201–99499), surgery (10021–69990), imaging (70100–79999), and therapy (97000 series), depending on the procedure performed.






.webp)