Upcoding And Downcoding: Key Differences, Risks & Prevention
Learn the differences between upcoding and downcoding in medical billing. Understand financial impacts, legal risks, and how AI ensures coding accuracy.
October 21, 2025


Key Takeaways:
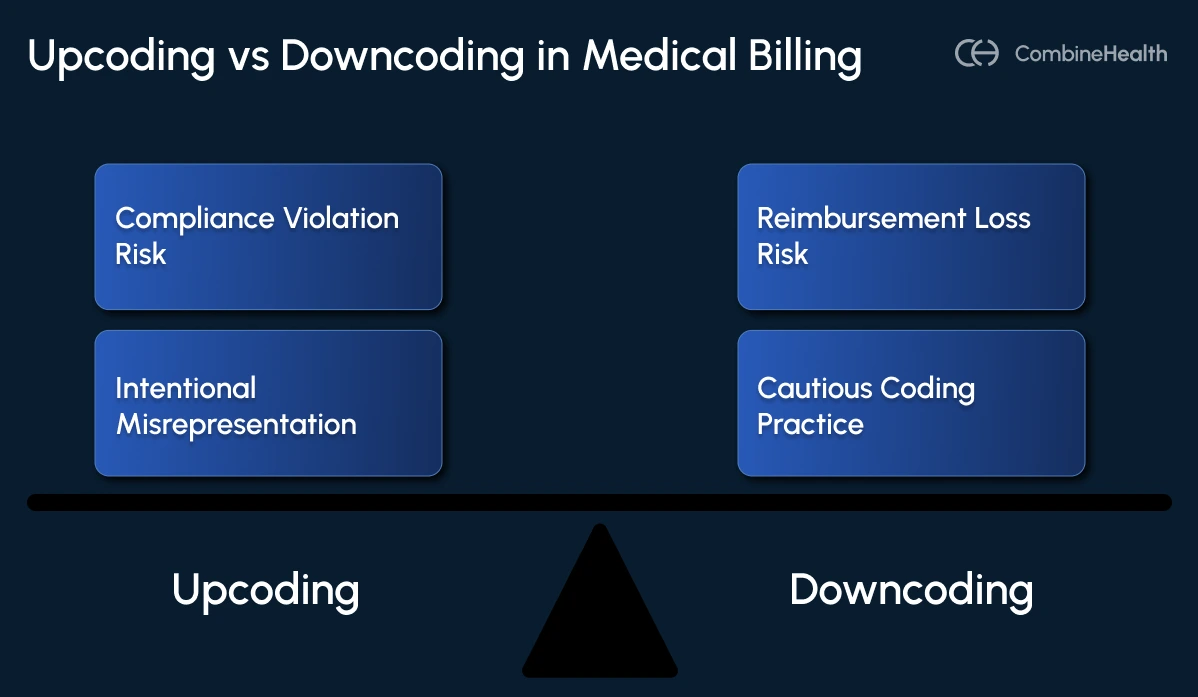
• Upcoding bills for higher services (fraudulent), while downcoding bills for lower services (revenue loss).
• Downcoding costs 10-30% revenue; upcoding risks $250k fines and imprisonment.
• Downcoding stems from poor documentation; upcoding typically involves intentional fraud.
• AI tools automate coding and audits; prevention requires routine audits, training, and checklists.
In medical billing, when codes don't match services, healthcare organizations turn to two opposite but equally damaging workarounds.
First is upcoding, which illegally inflates revenue, and the second is downcoding, which legitimately strangles it. For financial leaders watching their top line, understanding this distinction is crucial for survival.
For individual organizations, downcoding alone can cause revenue losses of 10-30%, potentially reaching $125,000 annually for many providers. Meanwhile, upcoding violations can bring fines up to $250,000 and imprisonment for up to five years per incident.
What Is the Difference Between Upcoding and Downcoding?
While both upcoding and downcoding represent mismatches between services provided and codes billed, they stem from different causes, create different problems, and carry different risks.
Upcoding: The Fraudulent Overbilling Practice
Upcoding occurs when healthcare providers submit billing codes for diagnoses, procedures, or services that are more serious, complex, or time-consuming than what was actually provided. This practice deliberately inflates claims to receive higher reimbursement from insurance companies or government programs.
Common examples of upcoding include:
- Billing for a comprehensive examination when only a basic evaluation was performed
- Using codes for new patients instead of established patients (which pay at higher rates)
- Billing for 60-minute psychotherapy sessions when only 30 minutes of service were provided
- Misrepresenting surgical procedures as more complex than they actually are
- Adding unnecessary diagnostic codes to justify higher-level billing
Primary causes: Typically, intentional fraud, though sometimes it results from inadequate documentation that doesn't support the higher-level code selected.
Downcoding: The Revenue Loss Problem
Downcoding refers to assigning medical billing codes that reflect a lower level of service or treatment than what was actually provided. This practice results in reduced reimbursement for healthcare providers and typically occurs due to insufficient documentation, payer adjustments, or conservative billing approaches.
Common examples of downcoding include:
- A comprehensive examination being processed as a limited exam due to inadequate documentation
- Level 4 office visits (CPT 99214) being reduced to Level 3 (CPT 99213) by payers
- Complex surgical procedures being billed at basic procedure rates due to incomplete operative notes
- Anesthesia services being reimbursed for fewer time units than actually provided
Primary causes: Typically unintentional—resulting from insufficient documentation, overcautious coding practices, or payer-initiated adjustments during claims processing.
Consequences of Upcoding and Downcoding
Upcoding isn't just a billing error—it's a federal crime that can trigger massive fines, prison time, and exclusion from Medicare and Medicaid.
Legal and Compliance Impact
The legal consequences of upcoding are severe and can devastate healthcare organizations. Under the False Claims Act, violations can result in fines up to $250,000 and imprisonment for up to five years. Civil penalties range from treble damages plus fines of $13,508 to $28,619 per false claim.
Upcoding violates multiple federal statutes, primarily the False Claims Act (FCA), which prohibits knowingly submitting false claims to federal healthcare programs. The legal framework includes criminal charges (up to 5 years imprisonment and $250,000 fines), civil penalties (treble damages plus per-claim fines), program exclusion from Medicare and Medicaid, and potential license revocation and professional sanctions.
Recent enforcement examples show the severe consequences:
- CareAll Management LLC paid $25 million for upcoding home health billings
- EndoGastric Solutions returned $5.25 million for device upcoding violations
- NextCare Inc. paid $10 million for inflated urgent care procedure billing
While downcoding isn't typically fraudulent, it creates compliance risks through potential audit triggers. Regulatory bodies may investigate patterns of underbilling as potential indicators of systemic billing problems or attempts to avoid scrutiny.
Revenue Impact
Industry statistics show the pervasive revenue impact:
- Approximately 8-10% of claims are affected by downcoding
- Revenue losses of 10-30% due to coding inaccuracies
- Potential annual losses reaching $125,000 for many providers
- Downcoding incidents have increased with recent ICD-10 updates
For a typical 20-provider clinic, these downcoding losses can represent $100,000+ in missed revenue annually—funds that could have been invested in new equipment, staff development, or practice expansion.
Reputation Damage
Beyond immediate financial impacts, both coding practices damage the provider's reputation. Upcoding investigations become public, eroding patient trust and referral relationships. Downcoding patterns may signal incompetence to payers, leading to increased audit frequency and more aggressive claims scrutiny.
Patients affected by downcoding often face higher out-of-pocket costs when their claims are processed at lower levels than appropriate, leading to dissatisfaction and potential practice switching. The administrative burden of addressing patient billing complaints further strains staff resources and damages the practice's reputation.
Detecting and Preventing Upcoding and Downcoding
A structured audit program proactively identifies coding discrepancies, protecting your organization from both financial losses and compliance penalties.
Conduct Routine Internal Audits and Peer Reviews
Regular internal audits are your first line of defense against both upcoding and downcoding. These should include:
- Pre-bill audits: Reviewing coded claims before submission to catch errors early
- Random chart reviews: Selecting a representative sample of encounters for detailed coding validation
- Provider-specific analysis: Identifying individual patterns that may indicate systematic issues
- Peer comparison: Benchmarking coding patterns against similar providers and specialties
Train Providers on Documentation That Supports Medical Necessity
Clinical documentation is the foundation of accurate coding. Without detailed notes that justify the complexity of care provided, even appropriate coding may be downcoded by payers. Effective training should focus on:
- Specificity: Documenting precise diagnoses rather than general symptoms
- Medical decision-making: Clearly capturing the complexity of clinical reasoning
- Time documentation: Accurately recording time spent when time-based coding applies
- Comprehensive exam documentation: Ensuring all elements are properly captured and described
Use Compliance Checklists (E/M Leveling, Modifier Validation, etc.)
Standardized checklists ensure consistent coding practices across your organization. These should include:
- E/M leveling criteria: Clear guidelines for each level of service based on documentation elements
- Modifier validation: Rules for appropriate modifier usage with examples of common misapplications
- Documentation requirements: Specific elements needed to support each code level
- Payer-specific rules: Checklists tailored to major payers' unique requirements
Maintain Audit Trails for Every Code Change
Complete transparency in coding decisions is essential for both compliance and revenue optimization. Your systems should capture:
- Original codes selected: The initially assigned codes before any changes
- Rationale for changes: Specific reasons for code modifications
- Documentation references: Links to clinical notes supporting coding decisions
- Staff involved: Who made coding decisions, and any reviews conducted
- Timestamps: When codes were assigned, reviewed, and modified
These audit trails not only support compliance but also identify patterns that may indicate needed education or process improvements.
How AI Coding Agents Can Help
Traditional approaches to coding accuracy rely heavily on human vigilance—but even the most experienced coders struggle against constantly changing payer rules, documentation variations, and the sheer volume of claims. This is where AI Medical Coding Agents transform the equation.
AI Medical Coding Agent like Amy from CombineHealth deliver 99.2%+ coding accuracy by combining deep medical coding knowledge with continuous learning capabilities. Our specialized AI agents address both upcoding and downcoding challenges through several key capabilities:
Real-time Documentation Analysis: Our AI Agents read encounter notes directly from EMRs, applying comprehensive coding guidelines including ICD-10, CPT, HCPCS Level II, E/M, Modifiers, and HCC. They flag documentation gaps such as incomplete procedure details, missing findings from independent interpretation, or unsupported diagnoses while the encounter is still in progress.
Explainable Decision-Making: Unlike black-box AI solutions, our AI Medical Coding Agent provides line-by-line rationale and evidence behind each coding decision. This transparency allows human reviewers to understand exactly why specific codes were selected, creating natural audit trails and supporting education.
Payer-Specific Rule Compliance: Our AI Agents incorporate continuously updated rules across 50+ different payer guidelines, automatically applying the specific requirements of each payer to minimize denials and downcoding.
Proactive Error Prevention: By analyzing patterns across thousands of claims, our AI Agents identify systemic coding issues before they create widespread problems. They can audit pre-coded charts to highlight potential upcoding risks or undercoding patterns, allowing proactive correction.
Continuous Learning from Denials: AI denial management specialists like CombineHealth’s Adam learn from prior denial patterns to prevent future occurrences.
Ensure Coding Accuracy With CombineHealth
Both upcoding and downcoding require proactive management through technology, training, and systematic compliance programs to protect organizational financial health and regulatory standing.
The solution lies in a specialized agentic AI workforce that can maintain coding accuracy while providing complete transparency into decision-making. This approach addresses both the compliance risks of upcoding and the revenue leakage of downcoding, turning coding accuracy from a persistent challenge into a measurable advantage.
Book a demo with CombineHealth today!
FAQs
What is upcoding and downcoding in medical coding?
Upcoding involves billing for higher-level services than actually provided, typically resulting in fraudulent overpayment. Downcoding involves billing for lower-level services than provided, resulting in legitimate revenue loss and operational inefficiencies.
Can downcoding increase reimbursements?
No, downcoding consistently reduces reimbursements by billing at lower levels than justified by the services provided. It represents a lost revenue opportunity rather than any financial benefit.
Why should we avoid upcoding?
Upcoding carries severe legal consequences, including fines up to $250,000, imprisonment up to five years, treble damages under the False Claims Act, program exclusion from Medicare/Medicaid, and potential license revocation.
How can you avoid accidentally upcoding?
Implement robust compliance programs, including regular staff training, clear coding policies, automated coding software with built-in compliance checks, routine reviews of billing patterns against peer benchmarks, and segregation of duties in billing processes.
Is downcoding illegal?
Downcoding itself typically isn't illegal unless done systematically to avoid scrutiny, but it violates coding integrity principles and causes significant revenue loss. The National Correct Coding Initiative requires physicians to use the most comprehensive code supported by documentation.






.webp)