Top 10 AI Medical Coding Solutions for 2026
Explore our top picks for ten best AI coding solutions for 2026 that RCM teams should check out to increase their reimbursement and reduce coding-related claim denials.
December 16, 2025


Key takeaways:
• Coding errors cost U.S Healthcare organizations more than $125 billion annually due to coding errors.
• AI Medical Coding solutions can improve accuracy, speed, compliance, and revenue integrity.
• This curated list of Top 10 AI Medical Coding solutions is built by experts with over 50+ years of combined experience in revenue cycle management and AI.
• The best AI Medical Coding solution for 2026 is Amy by CombineHealth, which leads in accuracy, explainability, automation, and enterprise-grade integrations.
Healthcare providers are spending upwards of $20 billion to overturn denied claims due to coding inaccuracies, missing documentation, and compliance gaps. The market is now flooded with “AI coding solutions”, all promising unmatched accuracy and automation. But which coding tools actually deliver?
Our RCM and AI experts have curated a list after weeks of research to review the most trusted AI medical coding platforms to produce the definitive list for 2026.
Why AI Adoption Is Important in Medical Coding
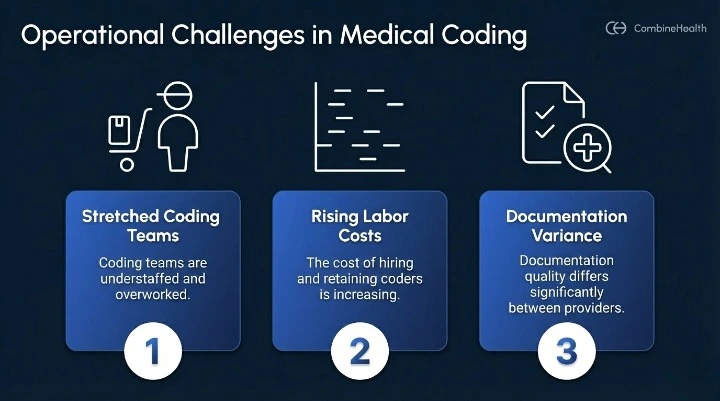
AI medical coding has become essential because healthcare organizations are facing real operational pressure.
- Coding teams are stretched thin
- Labor costs keep climbing
- Documentation varies widely from provider to provider
These issues lead directly to high denial rates and slow turnaround times, which ultimately impact cash flow and revenue integrity. At the same time, regulatory requirements continue to evolve, including ICD-10, CPT updates, LCDs, NCDs, and payor-specific rules, making it harder for human coders to keep pace consistently.
According to Black Book Research, more than 70 percent of health systems plan to expand AI-driven automation in their revenue cycle by 2026, with autonomous medical coding at the top of the priority list. Organizations are looking for technology that can reduce manual workload while improving accuracy and compliance.
Modern AI coding platforms are already delivering measurable improvements. Many health systems are seeing a 30 to 70 percent reduction in coding-related FTE workload, coding cycles that move 50 percent faster, and denial rates that drop by 20 to 40 percent once AI is fully integrated.
How Is AI Used in medical coding?
AI is used in medical coding for:
- Reading clinical documentation
- Understanding the clinical context
- Assigning accurate ICD-10, CPT, and HCPCS codes
- Intelligently scrubbing claims
- Clinical documentation improvement
- Auditing
Instead of relying on fixed rules like older CAC systems, modern AI uses natural language processing and large language models to interpret provider notes the way a trained coder would, checking medical necessity, NCCI edits, and payor policies along the way.
What’s new for 2026 is the rise of agentic AI technology. Unlike traditional CAC-based coding, today’s AI systems do more than make suggestions. They can also:
- Plan tasks
- Reason through coding guidelines
- Act across different RCM applications
- Improve based on feedback
In practical terms, they operate like an AI employee that autonomously reviews charts, extracts key clinical details, assigns codes with clear explanations, and flags cases that need human oversight.
This shift allows organizations to handle higher coding volumes, reduce errors, and maintain compliance without adding more manual workload.
Top 10 AI Medical Coding Solutions for 2026
1. Amy - AI Medical Coding solution by CombineHealth (Top Rated for 2026)
CombineHealth’s Amy AI is the most advanced AI medical coding solution in the U.S. market for 2026. It delivers fully explainable code recommendations with payor policy references and audit trails. It integrates directly with major EHRs, clearinghouses, and RCM workflows.
Why Amy AI Stands Out?
Amy AI offers an auditable explanation for every code she assigns, which helps coding teams and compliance leaders maintain confidence in the results.
Key Features
- Autonomous medical coding across 30+ specialties
- Policy-backed rationale for every recommendation
- Modifier logic, NCCI edits, LCD/NCD checks
- Human-in-the-loop review workflows
- Seamless integration with Epic, Cerner, Athena, eCW, NextGen, and others
- High accuracy validated across millions of encounters
- Audit trail for compliance
Best use case for
- Mid-size to large-size provider hospitals
- Multi-specialty groups and Health systems
- Physician groups and ASCs

2. Optum Integrity One by Optum
Optum’s Integrity One is a coding and documentation platform that combines rules-based logic with machine learning to support accurate coding, documentation review, and compliance oversight. It’s suitable for large health systems and RCM organizations that require structured governance and audit capabilities.
Key Features
- Rules-driven and ML-assisted coding checks
- LCD/NCD and payor policy validation
- CDI support and audit workflows
- Revenue integrity reporting and analytics
Best use case for:
- Large enterprises focusing on compliance and standardised review process
- Mid-size hospitals and groups
3. Infinx
Infinx providers AI medical coding solution to increase clean claim submission rate and reduce coding-related denials with complex coding services enabled by the latest technology. It leverages Maverick’s mCoder™to deliver an 85% direct-to-bill rate and reduce coding errors with proprietary deep learning AI.
Key features
- Automated code generation using NLP and ML
- Support for ICD-10-CM, CPT, HCPCS, and modifiers
- Real-time coding validation and compliance checks
- Reporting tools for accuracy, productivity, and audit review
Best use case for:
- Hospitals and mid-size RCM teams
- Physician groups and practices
4. Solventum™ 360 Encompass™
Solventum (formerly part of 3M Health Information Systems) offers an AI-supported medical coding platform built on their expertise in clinical documentation, CDI, and coding workflows. The solution uses NLP, machine learning, and a comprehensive rules engine to assist coders with accurate and compliant code assignment across inpatient and outpatient settings.
Key features
- NLP-driven clinical documentation interpretation
- ICD-10, CPT, and HCPCS code support with real-time validation
- Integrated CDI workflows and documentation improvement prompts
- Coding edits and compliance logic aligned with national guidelines
Best use case for:
- Hospitals and health systems
5. TachyHealth
TachyHealth delivers an AI-powered revenue cycle management platform that automates medical coding and denial prevention across specialties like orthopedics, using advanced deep learning, clinical NLP, and vast datasets from leading health systems.
The solution drives autonomous or near-autonomous coding with high accuracy, fueled by ongoing model refinement and specialty-tuned logic.
Key features:
- Automated ICD-10, CPT, and HCPCS code generation
- Specialty-specific AI models trained on real clinical data
- Continuous learning from coder feedback and documentation patterns
- Real-time compliance validation and audit-ready outputs
Best use case for:
- Hospitals
- Academic Medical Centers
- Multi-specialty Groups
6. Exdion Health
Exdion Health delivers an autonomous medical coding platform powered by deep learning, large language models, and vast clinical datasets to produce complete, audit-ready codes.
The solution enables high-speed, high-volume coding for organizations seeking to slash manual workloads and boost coding consistency through intelligent revenue intelligence.
Key features
- E&M level validation based on documentation
- Review of modifier usage
- Claim Scrubbing based on CCI edits, HCPCS and other standard guidelines
- Reporting that helps isolate provider training needs, code level detail
Best use case for:
- Billing companies
- Urgent Care Providers
7. PCH Global
PCH Health's AI coding platform provides automation and advanced decision-making tools, streamlining mid-revenue cycle and central billing processes. It automates CPT codes, diagnoses, HCPCS codes, E/M levels, and charges.
The AI medical coding solutions integrate seamlessly with expert human oversight to deliver customized services, empowering healthcare providers with advanced AI, enhanced workflow efficiency, and supplementary coding support for consistent, scalable results.
Key features:
- Fully transparent audit trails
- Real-time reporting and analytics
- Seamless integration with major EHRs
- Scalable global operations for large-volume coding support
Best use case for:
- Health systems
- Physician groups
8. AGS Health
AGS Health provides an AI-powered medical coding platform that blends advanced NLP, machine learning, and a large team of certified coders to streamline clinical abstraction and code assignment.
Their solution uses emerging technologies such as ML, NLP, clinical language understanding (CLU), computational linguistics, knowledge graphs, and large language models (LLMs) to make coding processes more efficient.
Key features:
- Autonomous coder combined with coding services
- Automated documentation review and compliance checks
- Seamless integration with major EHR and billing systems
- Scalable global delivery model for high-volume coding programs
Best use case for:
- Health systems
9. IKS Health
IKS Health’s medical coding platform leverages advanced artificial intelligence to streamline documentation review and accelerate coding accuracy. Using NLP and machine learning, the platform autonomously extracts key clinical details from patient charts and recommends ICD-10, CPT, and HCPCS codes, reducing manual effort and improving coding consistency.
Key features:
- Fully-managed and flexible coding solutions with AAPC, AHIMA-certified coders
- Flexible staffing services
- Auditing and compliant coding
- Clinical documentation improvement
Best use case for:
- Specialty Clinics
- Ambulatory Centers
- Physician Practises
10. athenaOne by AthenaHealth
athenaOne, Athenahealth’s integrated practice management and EHR platform, incorporates AI-assisted medical coding to streamline documentation review and support accurate code assignment. The system uses NLP and rule-based logic to interpret clinical notes, surface coding suggestions, and reduce administrative workload for providers and coders.
Key features:
- Automated code recommendations
Documentation analysis to flag missing or incomplete elements - Continuous regulatory updates aligned with payor and coding changes
- Seamless integration with scheduling, EHR, and billing functions across the athenaOne suite
Best use case for:
- Physician practises
- Ambulatory groups
How To Choose the Right AI Medical Coding Solution
Choosing the right AI medical coding solution starts with a clear understanding of your organization’s operational realities and long-term goals. Before comparing vendors, it is essential to map your coding volume, specialty mix, workflow gaps, and integration requirements. From there, evaluating vendor maturity and anticipating implementation challenges will help ensure you select a solution that delivers measurable ROI.
Assess Your Organization’s Needs
Before selecting an AI Medical Coding Solution, it helps to ground the decision in a structured evaluation framework. The entire process often involves juggling multiple stakeholders, clinical leaders, IT, compliance, and revenue cycle operations, so starting with a unified checklist ensures alignment from the beginning. By clarifying internal needs, operational constraints, and readiness for automation, teams can quickly narrow down vendors that truly fit their environment rather than relying on marketing claims. Below is a practical checklist your procurement team can use to guide the evaluation process.
- Coding volume (daily, monthly, specialty mix)
- Specialty-specific requirements
- Accuracy, speed, or denial-related pain points
- In-house vs outsourced operating model
- Integration requirements
- Implementation timeline tolerance
- End-user training needs
- Budget and expected ROI
Evaluate the Vendors
Evaluating the vendor is one of the most critical steps, especially for organizations looking for long-term system reliability and regulatory alignment. Beyond product demonstrations, it is essential to understand the company behind the technology, its level of customer support, AI engineering expertise, compliance approach, and overall stability. A structured evaluation helps ensure you select a partner that can keep pace with regulatory changes, maintain high accuracy, and provide dependable support throughout the lifecycle of the solution. Below is a checklist you can use to assess vendor strength and fit.
- Customer support quality
- Company stability and reputation
- Security and compliance (SOC 2, HIPAA)
- Medical coding expertise
- AI engineering capabilities
Further Reading: Tough question to ask when assessing an AI RCM coding solution
Create an Implementation Plan
AI Medical Coding implementations often succeed or struggle based on how well an organization prepares for operational and workflow disruptions. Even strong platforms require structured onboarding, integration of coding grid and payor-specific guidelines, documentation cleanup, and thoughtful change management. Understanding the most common challenges up-front helps set realistic expectations and ensures smoother adoption across clinical, coding, and billing teams.
Common Implementation Challenges to Anticipate
- Provider documentation variability that affects model accuracy and completeness
- Resistance from coders, clinicians, or operations teams adjusting to new workflows
- EHR or legacy system limitations that restrict integration or data availability
- The need for initial model calibration, accuracy tuning, and feedback loops
- Continuous updates to coding guidelines, payor rules, and compliance policies
Define ROI
Understanding the potential return on investment is essential for you to make a business case for AI Medical Coding. ROI is not only about reducing costs, it also includes operational efficiency, revenue integrity, and the downstream impact on denials and cash flow. By quantifying baseline metrics and comparing them to expected improvements, teams can build a clear, defensible financial model that aligns with leadership expectations. Below are some metrics you can use to evaluate ROI drivers and determine whether a solution delivers meaningful value.
- Reduction in FTE workload
- Denial rate reduction
- Faster turnaround times
- Quality and accuracy improvement
- Increased revenue capture
.webp)
How to Implement AI Medical Coding Solution at your Organization
Implementing an AI medical coding solution is most successful when organizations take a structured, phased approach. Rather than deploying systemwide on day one, teams should focus on building confidence, validating accuracy, and creating strong collaborative workflows between coders, clinicians, and the vendor. The goal is to ensure the technology enhances existing processes while reducing risk and operational friction. Below is a practical, step-by-step guide to help your team implement AI coding effectively.
- Start with a pilot – Begin with one specialty, department, or encounter type to validate performance, understand workflow impact, and gather real-world data before expanding organization-wide.
- Secure staff buy-in – Offer clear communication, training, and transparency about how the AI supports coders rather than replaces them. Early buy-in reduces resistance and improves adoption.
- Establish baseline metrics – Document current accuracy, turnaround time, denial rates, and cost per chart. These benchmarks help measure the AI’s impact and justify expansion.
- Monitor accuracy during calibration – AI models often require a short calibration period. Continuous monitoring ensures discrepancies are identified early and resolved with vendor support.
- Plan for guideline updates – Coding rules evolve frequently. Confirm your vendor updates models regularly and has strong governance processes to stay compliant.
- Maintain human oversight – Keep coders involved, especially for complex encounters or edge cases. Human review ensures quality and provides feedback that improves the AI over time.
- Scale gradually – As accuracy stabilizes and workflows mature, expand the AI solution to additional specialties and encounter types to capture full operational value.
To see how a fully autonomous, audit-ready workflow operates in real RCM environments, you can book a demo with CombineHealth. Their AI medical coding solution, Amy, delivers high accuracy, deep explainability, seamless EHR integration, and compliance-first automation—helping organizations reduce operational costs, improve revenue capture, and eliminate coding backlogs with confidence.
FAQs
How accurate are AI medical coding solutions?
Most leading platforms deliver 92–99.2%+ accuracy, with performance improving as different AI models adapt to specialty nuances and documentation patterns.
Can AI replace medical coders?
No, AI automates routine coding, but human coders remain essential for complex cases, compliance review, and continuous quality assurance.
How does explainable AI build trust in automated coding?
Explainable AI shows why each code was assigned by highlighting clinical context and rules, helping coders and auditors verify accuracy with confidence.
How long does implementation usually take?
Most deployments take 2–12 weeks depending on EHR integrations, data readiness, and workflow customization.
How do I choose the right AI medical coding vendor?
Look for strong accuracy benchmarks, specialty depth, compliance certifications, transparent outputs, and proven integration with your billing and EHR systems.





.webp)

