Trauma Coding 101: How to Capture Every Dollar and Avoid Costly Misses
Learn the essentials of trauma coding, activation billing, and RCM strategies to reduce denials, prevent revenue leakage, and capture every earned dollar.
December 18, 2025


Key Takeaways:
• Trauma coding is complex and often underpaid. Missed activation charges, injury details, and critical care time lead to major revenue leakage.
• Trauma ≠ critical care coding. Trauma billing hinges on EMS pre-notification, activation levels, and injury mechanisms, not just time-based care.
• Trauma center level directly limits what you can bill. You can’t bill higher activation codes than your state/ACS designation allows.
• Most trauma RCM breakdowns come from documentation gaps and staffing pressure. High acuity + shortages = higher denials and delays.
• AI helps close the gap. Real-time documentation, automated coding, and proactive denial management protect revenue without slowing care.
Trauma care never stops. It runs around the clock, and is supported by expert teams, advanced equipment, and lightning-fast response systems that activate the moment EMS (Emergency Medical Services) calls in.
But despite this, trauma programs face a persistent challenge: revenue capture rarely reflects the true complexity of the care delivered. High-value services such as trauma activations, emergency surgeries, and multi-specialty care are often undercoded, under-documented, and underpaid, resulting in substantial financial loss.
Here’s a deep dive into the fundamentals and nuances of trauma coding—and the tools that help protect revenue, reduce errors, and avoid costly misses.
What Is Trauma Coding?
Trauma coding is the process of translating trauma-related injuries, procedures, and activation services into accurate ICD-10-CM diagnosis codes, CPT procedure codes, and trauma activation codes to ensure precise charge capture, payer reimbursement, and quality reporting.
The Key Components of Trauma Coding
Below is a high-level overview of the key components of trauma coding:
How Is Trauma Coding Different From Critical Care Coding?
Although trauma and critical care often overlap clinically, they are distinct in both coding and billing.
Trauma coding focuses on injury-specific diagnoses caused by external events and may include critical care CPT codes when time and severity criteria are met during a trauma response.
Critical care coding, by contrast, applies to any imminent, life-threatening deterioration of vital organ systems, such as sepsis, cardiac arrest, or post-operative complications, and does not require a trauma mechanism. Here’s how they differ:
What Are The Challenges In Trauma RCM?

Trauma Revenue Cycle Management (RCM) is one of the most complex areas in healthcare billing and is especially vulnerable to errors, delays, and denials. Here’s what makes trauma RCM challenging:
- Extensive documentation: Trauma care demands meticulous, chronological documentation—from prehospital arrival through the ED, imaging, procedures, ICU, and disposition—to support accurate reimbursement, legal clarity, audit defense, and regulatory compliance.
- Multi-layered complex coding and billing: Trauma coders must work across code sets within a single case to capture trauma activation, multiple injuries, and services delivered by different providers. With so many moving parts, coding errors are far more likely.
- High denial rates: Trauma cases are time-sensitive and prioritize saving lives, which increases the risk of denials due to missing injury details, activation criteria, or critical care time. Trauma claims also face intense payer scrutiny, especially regarding activation levels, medical necessity, and critical care documentation.
- Staffing shortages: The demand for 24/7 trauma coverage collides with a shrinking healthcare workforce. A recent study revealed that nearly eight in ten Level I and II trauma centers face acute care surgeon shortages, creating pressure on both clinical and RCM performance.
- High operational costs: Trauma centers must maintain 24/7 readiness with on-call teams of highly experienced clinicians, specialized equipment, consumables, and continuous emergency support infrastructure. Sustaining these resource-intensive services is financially demanding.
What Are The Different Levels In Trauma Centers?
Trauma centers are classified into specific levels depending on their ability to care for injured patients.
Each center is designated a level (I–V) by the state government, based on clearly defined criteria related to staffing, resources, and clinical capabilities. Additionally, the American College of Surgeons (ACS) conducts a formal verification process to assess whether the trauma center meets national standards for trauma care.
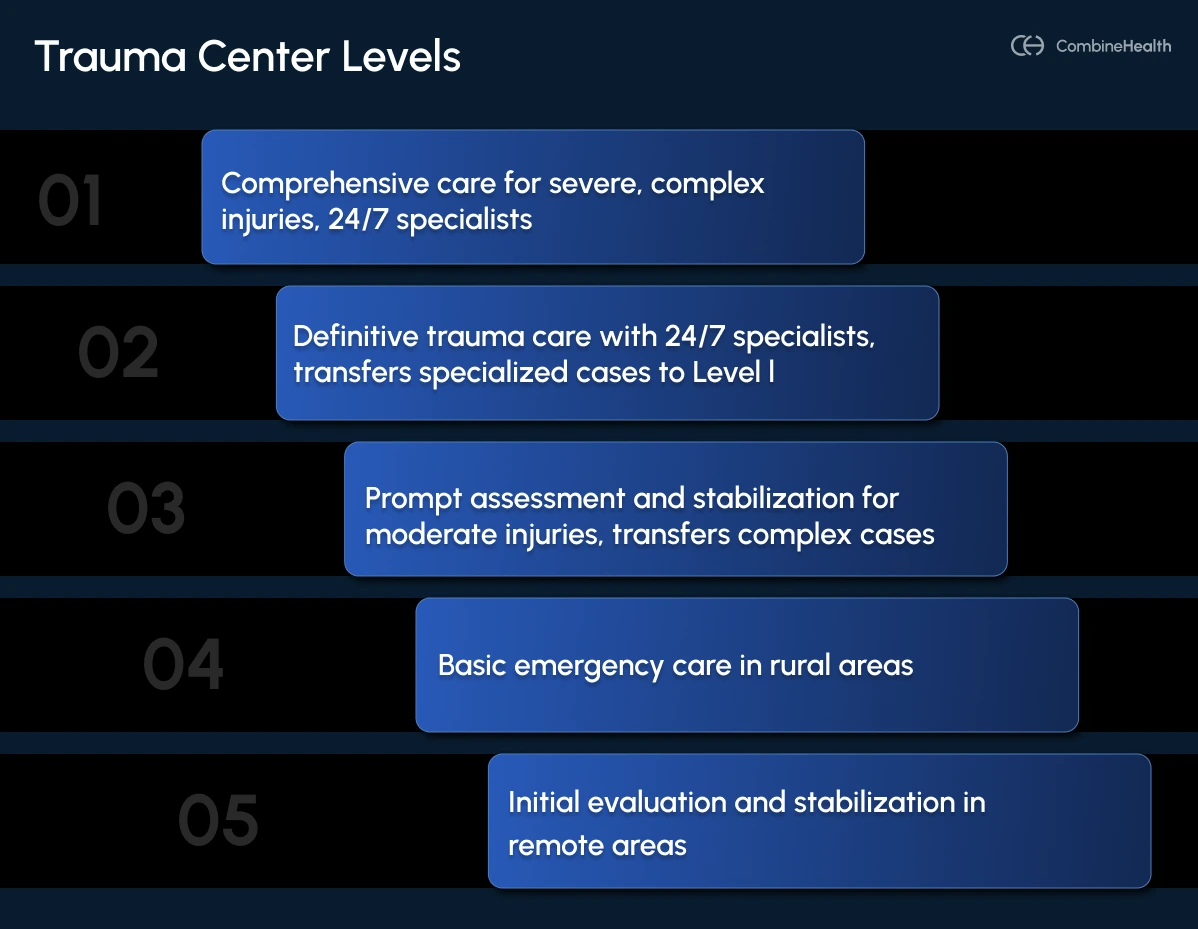
Below is a commonly accepted framework used to define trauma center levels:
Level I Trauma Center: For The Most Severe, Complex, And Multi-System Injuries
Level I trauma centers provide the highest level of trauma care, with 24/7 availability of trauma surgeons and all major specialists. They deliver comprehensive care across the entire continuum and are equipped to manage the most severe, complex, and multi-system trauma cases.
Example:
Treating a patient with polytrauma from a high-speed motor vehicle crash involving head injury, unstable pelvic fractures, internal bleeding, and multiple organ involvement
Level II Trauma Center: For Severe Injuries Requiring Definitive Care
Level II trauma centers are equipped to provide definitive trauma care, with clinical capabilities similar to Level I centers, including 24/7 availability of trauma surgeons and key specialists. They manage most severe trauma cases but may transfer highly specialized or resource-intensive cases, such as those requiring complex microvascular surgery, to Level I trauma centers.
Example:
Treating a patient with multiple long-bone fractures and internal injuries who requires urgent surgery but not specialized subspecialty care may be treated at a Level II trauma center
Level III Trauma Center: For Moderate Injuries Requiring Rapid Stabilization
Level III trauma centers provide prompt assessment, resuscitation, emergency surgery, and intensive care, supported by a 24/7 emergency medicine physician. They manage moderate trauma injuries and focus on rapid stabilization, transferring complex cases to Level I or Level II centers due to limited specialist availability.
Example:
Treating a patient with a stable abdominal injury or isolated head trauma who needs evaluation and possible surgical intervention may initially be treated at a Level III trauma center before transfer.
Level IV Trauma Center: For Basic Emergency Trauma Care
Level IV trauma centers deliver basic emergency trauma care, often serving rural or underserved areas. They maintain 24-hour laboratory and emergency services and are trained to provide Advanced Trauma Life Support (ATLS) before transferring patients who require higher-level trauma care.
Example:
Treating a patient with a suspected internal injury following a fall may be stabilized at a Level IV center before being transferred to a Level II or Level I trauma center.
Level V Trauma Center: For Initial Evaluation and Stabilization
Level V trauma centers provide initial evaluation and stabilization for injured patients, primarily in very remote or frontier regions. These facilities often have limited operating hours and focus on rapid assessment and transfer to higher-level trauma centers.
Example:
Treating a patient injured in a skiing accident in a remote mountain area may first receive stabilization at a Level V trauma center before being transferred to a higher-level trauma facility.
While trauma center levels define clinical capability, they also directly influence trauma activation criteria and how trauma services are billed. A hospital’s designation determines the trauma activation levels it can bill.
Let’s take a closer look at how this works:
What Is Trauma Activation and How Does It Work?
Trauma activation is the rapid mobilization of a specialized trauma team, including surgeons, anesthesiologists, emergency physicians, nurses, respiratory therapists, and ancillary staff, prior to the arrival of a severely injured patient.
It’s triggered when the hospital receives pre-hospital notification from EMS indicating that the patient meets specific injury, physiologic, or mechanism-of-injury criteria.
Once a trauma activation is triggered, the hospital launches a tiered response based on the patient’s condition, including vital signs, mechanism of injury (e.g., motor vehicle collision, fall, penetrating trauma), and visible signs of injury (e.g., head trauma, fractures, severe bleeding).
Most hospitals follow a three-tier trauma activation system:
Level 1 Activation (Full Activation/Code Red)
It’s the highest level of trauma response applicable to patients with unstable vital signs or clear life-threatening injuries.
Common triggers (physiologic & anatomic) include:
- Compromised airway or patient requiring intubation
- Systolic BP < 90 mmHg (adults) or need for blood products
- Glasgow Coma Scale ≤ 8, unconsciousness, or penetrating trauma to the head, neck, or torso
- Traumatic amputations above wrist/ankle, flail chest, unstable pelvic fractures
Level 2 Activation (Partial Activation/Code Yellow)
It’s the level of trauma response used for patients who are stable but have a mechanism of injury (MOI) associated with a high risk of serious internal injury. The goal is to assess the patient quickly before their condition worsens.
Common triggers (MOI) include:
- Falls >20 feet (adults) or >10 feet (children)
- Motor vehicle crashes involving high speeds (>40 mph), ejection, rollover, or death in the same compartment
- Pedestrian/bicyclist impact at speeds >10 mph
- Pregnant patients (>20 weeks) with abdominal trauma; patients on anticoagulants with head trauma
Level 3 Activation (Consult/Code Green)
Applicable for patients with lower-energy injuries who are hemodynamically stable but still require trauma evaluation or admission.
Common triggers include:
- Patient > 65 years of age
- Hip fractures
- Single-system injury or hypothermia
- Transfers from other hospitals
How To Bill For Trauma Activation?
Critical care on its own is reimbursed at a standard rate, but when it’s paired with a properly documented trauma activation, reimbursement increases significantly. That’s why accurate trauma activation billing is so critical.
Here’s how to get it right:
1. Fulfill the Core Requirements
To bill for trauma activation, you must meet two key conditions:
- Pre-hospital notification: The trauma team is activated based on information received from EMS (The notification time and source must be documented in the medical record).
- Organized response: A designated trauma team responds on the patient’s arrival.
2. Assign Accurate Trauma Codes
Trauma activation is billed on the UB-04 (CMS-1450) facility claim using revenue codes and HCPCS codes.
First, choose the revenue code that matches the level of trauma activation called:
- 0681 – Level I Trauma Activation
- 0682 – Level II Trauma Activation
- 0683 – Level III Trauma Activation
- 0684 – Level IV Trauma Activation
- 0689 – Other Trauma Activation (used in select states)
Key rules for applying trauma activation revenue code:
- When billing any 068x revenue code for trauma activation, you must typically set FL 14 (Type of Admission) to "5" (Trauma Center).
- If a patient walks in or is driven to the hospital without EMS notification, REV 068x should not be billed.
- A hospital cannot bill a trauma activation level higher than its designated trauma center level. For example, a Level II trauma center cannot bill Revenue Code 0681, even if they call a 'Level 1' activation for a critical patient. They must bill the code that corresponds to their own designation ceiling, i.e., 0682.
Here are a few billing examples:
Next, code for critical care services.
If a trauma activation includes at least 30 minutes of critical care, bill CPT 99291 (physician critical care) along with HCPCS G0390 (trauma response team).
However, if critical care is under 30 minutes, two scenarios arise:
- For Medicare: DO NOT bill G0390. The trauma activation fee (REV 068x) may not be reimbursed, but it should still be captured on your Cost Report to support a higher Case Mix Index (CMI).
- For Commercial payers: Many private payers, like the Blues, reimburse the trauma activation fee (REV 068x) without G0390 (depending on contract terms).
How Can AI Help Accelerate Trauma Care Reimbursements?
Trauma care reimbursement relies heavily on two pillars: documentation and trauma coding, and unfortunately, both are often unstable in fast-paced trauma environments.
A study on trauma care found that the mean accuracy, completeness, and overall quality of trauma coding were only 64.5%, 70%, and 67.5% respectively.
And that’s precisely where AI excels: delivering consistency and precision that’s impossible to achieve in high-pressure settings.
1. Real-Time Trauma Documentation
In the trauma bay, nurses or scribes race to capture events as they unfold, making errors almost unavoidable. AI medical scribes eliminate this burden.
For example, Jessica, CombineHealth’s AI Scribing Agent, captures the encounter in real time through voice-driven documentation and automatically formats it into an EHR-ready note that meets trauma-specific requirements.
With Jessica, your trauma teams can stay focused on saving lives, not scrambling to document them.
2. Automated Coding & Charge Capture
Trauma activations are often under-billed or miscoded due to missing details or coding complexity. AI fixes that by reading the clinical story as it unfolds.
Using advanced algorithms and NLP, AI can:
- Scan the EHR in real time
- Identify billable services
- Flag missing activation charges
- Pull key details from operative notes
- Suggest accurate diagnosis and procedure codes
For example, Mark, CombineHealth’s AI Billing Agent, auto-completes CMS-1500 and UB-04 forms and accurately captures every billable service.
Additionally, Amy, CombineHealth’s AI Coding Agent, spots documentation gaps and assigns precise ICD-10 and CPT codes with 99.2%+ accuracy, helping you secure maximum reimbursement while reducing audit risk.
3. Smarter Denial Management
Manual denial management usually drains staff productivity and slows down the entire revenue cycle. AI streamlines this process end-to-end.
Adam, CombineHealth’s AI Denial Management Agent, continuously monitors claim status, flags denials, and pinpoints their root cause. Adam actually makes phone calls, navigating IVRs, speaking with live agents, retrieving updates, and resolving issues without human intervention.
Next, Rachel, CombineHealth’s AI Appeals Management Agent, generates strong, evidence-based appeals that boost overturn rates.
Together, Adam and Rachel give you an always-on, fully automated denial recovery engine.
Improve Patient Care Without Sacrificing Your Healthcare Revenue
Trauma care is fast-paced; don’t let your revenue cycle fall behind.
Prime your trauma program for today’s challenges and tomorrow’s demands, and turn every encounter into a clinical and financial win.
Pair your world-class clinical team with our AI RCM agents and elevate performance across the board. Curious how this works? Let’s connect.
FAQs
1. What Is Trauma Coding?
Trauma coding is a specialized process of documenting and billing for trauma injury care. It involves coding for specific injuries (e.g., fractures), the external cause (e.g., a car crash), and the Trauma Activation—a unique fee (Revenue Code 068x) that covers the cost of assembling a standby medical team before the patient arrives.
2. Can a Level III Trauma Center bill for a Level I activation (0681)?
No. A hospital cannot bill for an activation level higher than its official designation. A Level III center is capped at billing Revenue Code 0683 or 0684, even if the patient is critically injured, because they are not staffed/verified to provide Level I resources.
3. Why Does My Claim Need "Type Of Admission 5" For Trauma?
"Type of Admission 5" flags the patient as a Trauma Center admission. Payers use this code to validate that your facility is a state-verified or ACS-verified trauma center eligible to bill activation fees. Mismatched codes (e.g., billing a trauma fee on a "Type 1 Emergency" admission) often trigger automatic claim denials.







