Top 10 AI Medical Coding Companies for the Emergency Department
Explore the top 10 AI medical coding solutions designed for the emergency department. Also, understand how to select the right AI medical coding vendor.
February 14, 2026


Key Takeaways:
• ED coding is uniquely complex and high-risk. Coders are expected to process ~120 charts per shift while managing evolving diagnoses, dual professional/facility rules, and heavy payer scrutiny.
• Generic AI tools fall short in the ED. Emergency departments require ED-specific logic for critical care, procedures, facility leveling, and audit defensibility.
• The right AI partner balances automation with oversight. Safe ED automation requires explainability, human-in-the-loop review, and strong governance—not blind auto-coding.
• Vendors vary widely. Some are AI-first, others services-led, and some are payer-side tools. Choosing the right fit depends on your ED volume, compliance risk, and internal resources.
• Successful ED AI mirrors experienced coders. It asks what happened, what resources were used, and what justifies the charges—escalating ambiguity rather than guessing.
Emergency department coding runs on extreme timelines.
According to AHIMA productivity guideline, ED coders are often expected to code around 120 ED encounters in an 8-hour day—roughly 15 charts an hour, or just four minutes per encounter.
Diagnoses evolve mid-visit, documentation comes from multiple clinicians, procedures and imaging are layered in real time, and payer scrutiny is highest where acuity is highest. Coders are expected to move fast and be perfectly defensible.
This is why AI medical coding has become essential in the emergency department and why generic outpatient tools fall short.
In this guide, we’ve compiled our top picks for the 10 best AI medical coding companies for the emergency department, while breaking down:
- What makes ED coding uniquely difficult
- How ED-ready AI actually works
- How to evaluate the top AI medical coding companies for emergency care
What Are the Common Challenges Faced by ED Medical Coders?
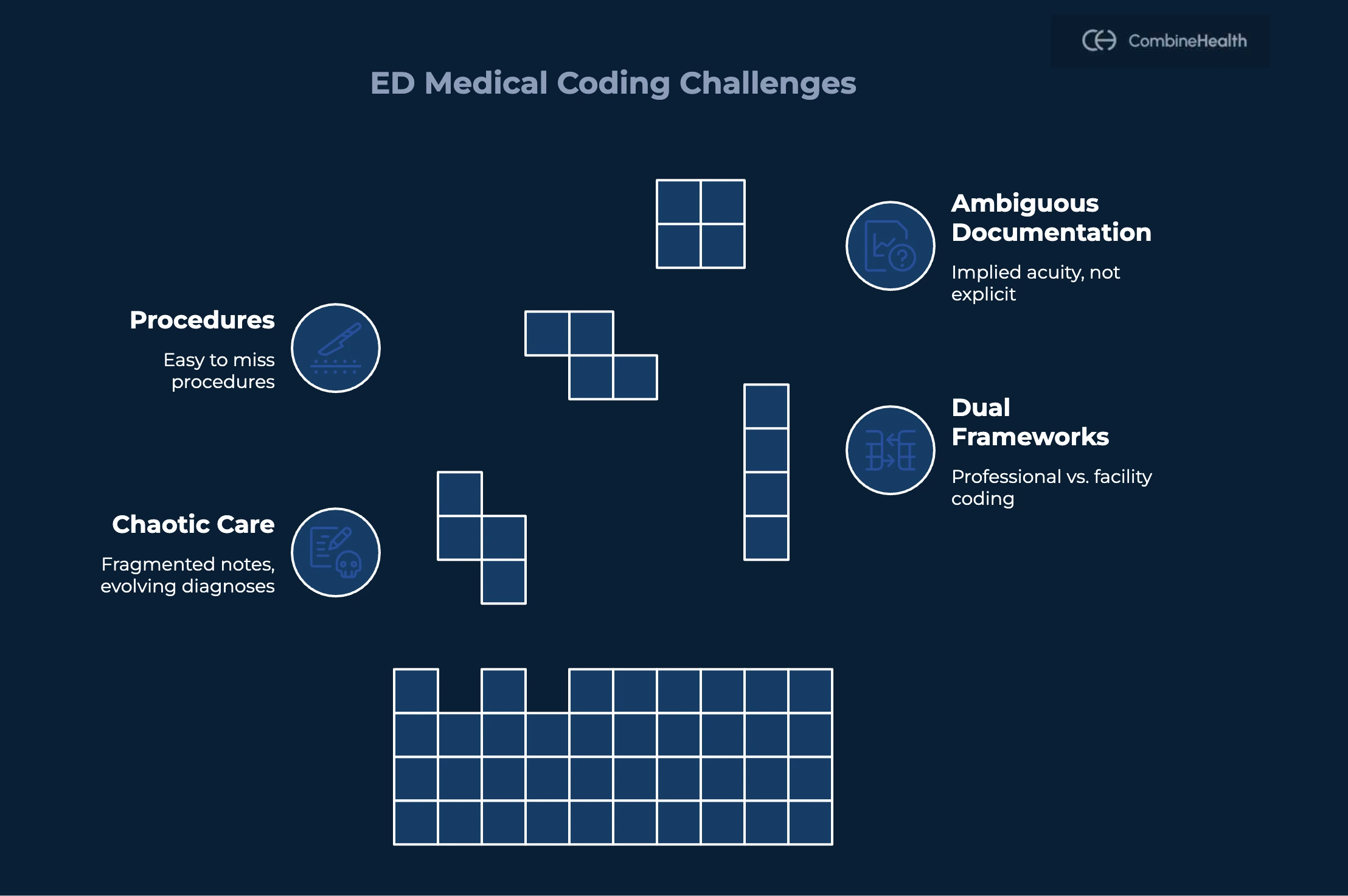
Emergency department medical coding comes with its own set of challenges, many of which don’t show up in other care settings. These often include:
Translating Chaotic ED Care into Structured Codes
ED visits rarely follow a clean narrative. Patients arrive without complete histories, diagnoses evolve over the course of the visit, and care is delivered across multiple handoffs.
Coders must reconstruct a coherent clinical story from fragmented provider notes, nursing documentation, lab results, imaging, and orders. When documentation is sparse, copied forward, or poorly organized, supporting higher-level E/M codes becomes especially difficult.
Plus, ED coders must stay fluent in constantly evolving E/M rules, particularly MDM-based leveling for CPT codes 99281–99285 and critical care services.
Navigating Dual Frameworks: Professional vs. Facility Coding
Most ED encounters generate two separate coding streams:
- Professional coding for the clinician, governed by CPT and MDM rules
- Facility coding for the hospital, driven by internal resource-based methodologies and payer-specific logic
These two levels frequently don’t align. Coders must reconcile discrepancies carefully—capturing appropriate revenue without introducing compliance risk or triggering audits.
Capturing Procedures and Add-on Services Accurately
Emergency clinicians perform a wide range of procedures—laceration repairs, splinting, I&Ds, procedural sedation, bedside ultrasounds, ECG interpretations—that are easy to miss in busy charts.
Coders must determine:
- Which procedures are separately reportable
- Which are bundled into the E/M codes
- When modifiers like -25 or -59 are appropriate
Ambiguous or Insufficient Documentation
In the ED, clinicians document to treat the patient, not to optimize billing. Moreover, ED volumes fluctuate unpredictably, creating coding backlogs and DNFB issues during peak periods. At the same time, many organizations face coder shortages and high turnover—especially among coders skilled in trauma, critical care, and pediatric ED cases.
As a result, acuity, complexity, and risk are often implied but not explicitly stated.
Coders are left choosing between:
- Under-coding, which protects against audits but sacrifices revenue
- Coding closer to clinical reality, which improves accuracy but may increase audit exposure
Provider queries can help, but they add friction and delay in an already overloaded environment.
Why Do You Need an AI Medical Coding Partner for the Emergency Department?
Once you understand how complex ED coding can get, the next question is obvious: how do you scale accuracy and speed without increasing risk? That’s where the right AI medical coding partner starts to matter.
Here’s why you need the right AI medical coding partner in an ED setting:
Revenue and Compliance Stakes are Higher
ED visits are a major revenue driver—and a top target for payer scrutiny. Payers apply ED-specific algorithms to down-code or reclassify visits as non-emergent.
High-risk scenarios like sepsis, chest pain, trauma, and stroke are common and heavily audited. Even small clinical documentation or coding gaps can trigger significant denials, recoupments, or compliance findings.
An ED-focused partner can tailor rules, edits, and audit trails to your payer mix and risk tolerance.
You Need Automation that Understands ED Nuance
ED-tuned AI can:
- Differentiate routine vs. complex encounters
- Identify true critical care
- Detect separately reportable procedures vs. bundled services
It can also align with local ED facility leveling guidelines, which is critical for accurate hospital reimbursement. Without ED-aware intelligence, automation tends to over-code (compliance risk) or under-code (revenue leakage).
An AI Medical Coding Partner Can Co‑Design Workflows with ED Reality in Mind
Successful AI adoption in emergency medicine depends on workflow design—not just model accuracy.
A dedicated partner can help define:
- What can be auto-coded vs. what needs review
- Exception handling for trauma and critical care
- Feedback loops between coders, clinicians, and AI
That level of co-design is hard to get from generic RCM tools or EHR add-ons.
Stronger Support for Denials, Appeals, and Audits
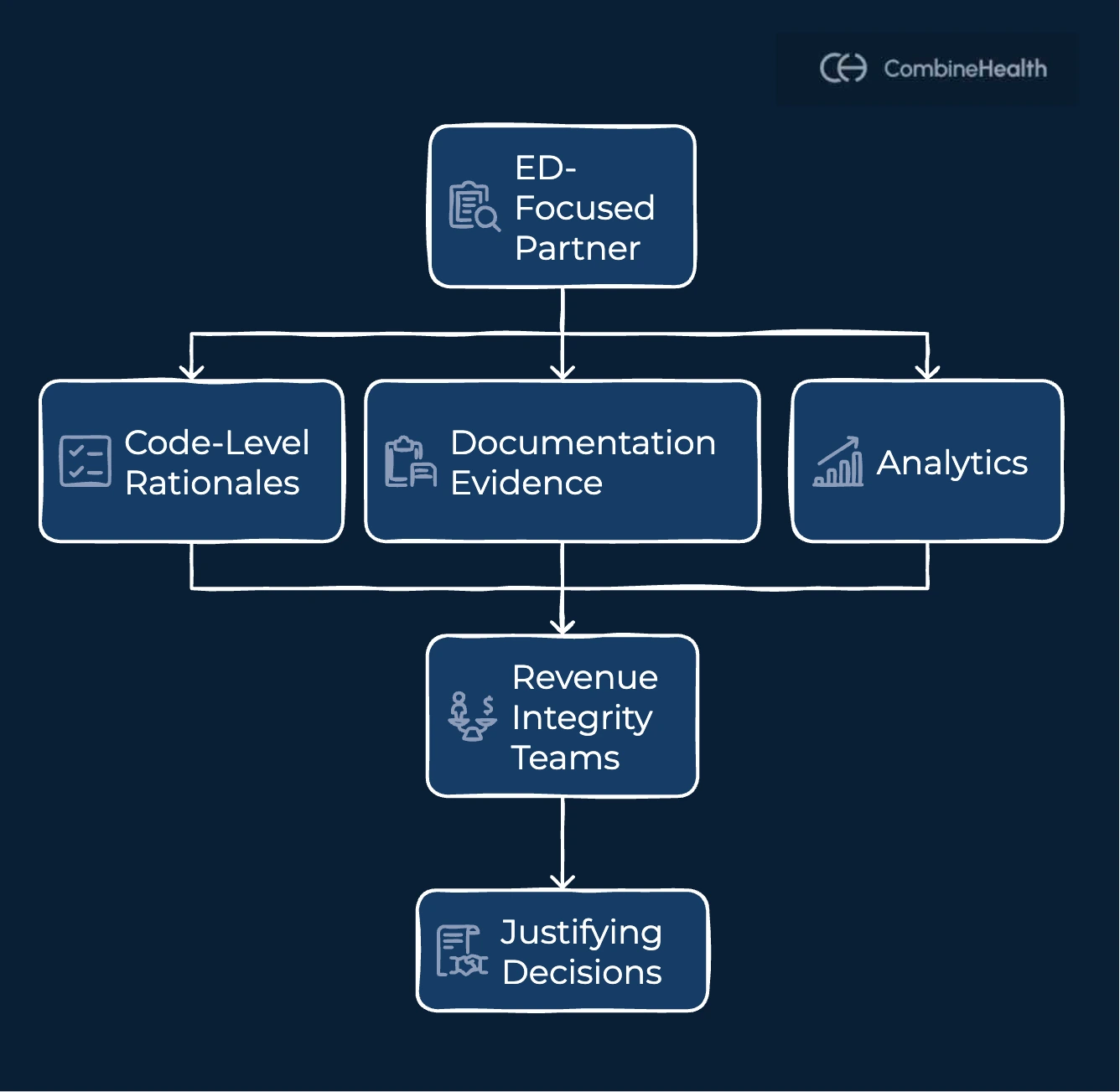
ED denials increasingly reference payer algorithms and clinical validation logic. You need explainable AI that shows why a code or level was assigned.
An ED-focused partner provides code-level rationales, documentation evidence, and analytics that help revenue integrity teams defend decisions—turning coding from a black box into a defensible system.
Scale Without Burning Out Your Team
ED coding teams face constant volume spikes and workforce strain.
An AI partner can handle routine, low-risk charts while experienced coders focus on complex cases, QA, education, and audit prevention. This balance improves throughput and retention, something in-house tools alone struggle to achieve.
10 Best AI Medical Coding Solutions and Companies for ED
1. CombineHealth: Best AI Medical Coding Solution for ED Specialties
CombineHealth provides ED-focused autonomous AI medical coding built for high-acuity, high-volume emergency departments. Its AI medical coding solution, Amy, mirrors expert coder reasoning, linking documentation, resource use, and payer rules.
The AI medical coding solution generates explainable, compliant professional and facility codes while scaling throughput without increasing audit risk.
Key Features:
- ED-specific AI medical coding for professional and facility E/M
- Strong support for critical care, trauma, imaging interpretation, and procedures
- Explainable AI with line-by-line coding rationale and audit trails
- Human-in-the-loop escalation for ambiguous or high-risk ED charts
- Payer-aware logic aligned with ED-leveling algorithms and medical necessity rules
- Integrated AI workforce covering coding (Amy), billing (Mark), denials, appeals, and policy review
Best For: Large Health Centers looking to scale ED coding while keeping human expertise central
Recommended Reading: How Emergency Medicine Has Evolved Over Time
2. Optum’s Emergency Department Claim (EDC) Analyzer
Optum’s Emergency Department Claim (EDC) Analyzer is a rules-based claim editing tool used primarily by payers to calculate and validate ED facility visit levels. It applies a CMS-aligned algorithm to diagnoses and procedures to estimate resource intensity and reprice ED facility E/M levels.
Key Features:
- Automated ED facility E/M leveling (99281–99285) using a weighted, multi-step algorithm
- CMS-aligned methodology based on outpatient facility E/M guidelines
- Assigns standard, extended, and patient-complexity weights to services and diagnoses
- Widely used for pre- and post-payment review and claim repricing
- Public-facing logic reference via EDCAnalyzer.com for transparency and testing
Best For: Provider organizations seeking to model payer behavior and understand how ED facility claims are scored
3. Logix Health
LogixHealth is a specialized RCM provider with more than 20 years of experience supporting emergency departments nationwide. Coding millions of ED visits annually, the company delivers end-to-end professional and facility coding, billing, and analytics designed to improve reimbursement, reduce denials, and scale high-volume ED operations.
Key Offerings:
- Full ED professional and facility coding, including E/M leveling, procedures, critical care, and quality reporting
- Claims management with denial prevention, appeals, and A/R follow-up
- ED-specific business intelligence dashboards tracking RVUs, charge capture, denials, and revenue trends
- Scalable RCM platform supporting millions of ED visits across multi-state operations
- Strong compliance focus with ongoing coder education and audit readiness
Best For: High-volume hospital EDs and emergency medicine groups needing end-to-end outsourced RCM
4. Edelberg & Associates
Edelberg & Associates is a U.S.-based medical coding and compliance firm specializing in emergency department, hospital, and multi-specialty coding.
Founded by nationally recognized coding expert Caral Edelberg, the firm helps organizations scale coding operations while maintaining strict compliance and audit defensibility.
Key Offerings:
- Turnkey professional and facility coding services, including ED and hospital medicine
- Web-based coding and audit platforms with queue management, productivity dashboards, and deep analytics
- Coding compliance audits, OIG and RAC audit defense, and denial support
- Provider education, documentation guidance, and ongoing feedback programs
- Flexible engagement models for backlog coverage, team augmentation, or point-of-service coding
Best For: Organizations facing audits or elevated denial risk that need a strong defense and reporting
5. AGS Health
AGS Health offers a hybrid AI-powered Autonomous Coding platform that combines advanced automation with human coding expertise. Designed for hospitals and health systems, it targets high-volume settings like emergency departments by automating routine coding while retaining human oversight for complex cases and compliance safety.
Key Features:
- Hybrid autonomous coding using ML, NLP, CLU, and LLMs with human-in-the-loop oversight
- Supports ICD-10-CM, CPT, HCPCS, modifiers, and E/M coding
- 40–80% automation potential in high-volume areas like ED and radiology
- Integrated compliance engine with NCCI edits, LCD/NCD logic, MCE, encoders, and pre-bill auditing
- Real-time dashboards for productivity, confidence scoring, suspends, RVUs, and acuity trends
Best For: Organizations seeking a hybrid AI + services model that integrates into existing RCM workflows
6. Medical Management Specialists
Medical Management Specialists (MMS), a division of ECS WMI, provides outsourced medical billing, coding, and practice management services. The firm emphasizes ethical billing, regulatory compliance, and documentation education to help physician groups optimize revenue while reducing administrative burden and operational risk.
Key Offerings:
- End-to-end RCM services including charge capture, CPT/ICD-10/HCPCS coding, claims submission, denial management, and collections
- Strong focus on documentation, education, and provider feedback to improve accuracy and reimbursement
- Practice management support with financial reporting and trend analysis
- Compliance-first approach aligned with evolving regulations and payer requirements
- Customizable engagement models for physicians and specialty groups
Best For: Small to mid-sized organizations wanting end-to-end RCM support without building internal teams
7. Zotec Partners
Zotec Partners offers Intelligent Coding through Z-Coder and Autocoder, an AI-driven coding platform built for high-volume emergency medicine groups. Trained on millions of ED encounters, it automates professional coding while routing uncertain cases to human coders to balance speed, accuracy, and compliance.
Key Features:
- ML-based Autocoder trained on millions of ED visits to predict CPT, ICD-10, E/M levels, modifiers, and MIPS codes
- 70–90% automation with confidence scoring and hybrid human review workflows
- Direct-to-billing for high-confidence cases; exceptions routed to coders
- TODAZ clinician feedback tool for real-time documentation gap identification and RFIs
- Real-time analytics for accuracy, TAT, denials, RVUs, and acuity trends
- Automatic updates for E/M guideline and regulatory changes
Best For: Hospital-affiliated ED providers focused on E/M optimization and denial reduction
8. Brault
Brault is a clinical intelligence and RCM partner focused on acute care physician groups, especially emergency medicine. Serving 4.2 million annual visits across 18 states, the firm combines AI-enabled workflows, U.S.-based nurse coding, and physician education to improve documentation, reduce denials, and optimize ED reimbursement.
Key Offerings:
- AI-enabled coding and billing for ICD-10, CPT, and E/M, supported by U.S.-based nurse and certified coders
- Clinical analytics and physician education programs to improve documentation and MDM optimization
- Practice management tools, including chart capture, payer contract management, and patient engagement
- Proactive denial monitoring, compliance training, and MIPS/QCDR quality reporting
Best For: Independent emergency medicine and hospitalist groups seeking clinically driven RCM support
9. Exdion Health
Exdion Health is an AI-powered RCM platform focused on ambulatory, urgent care, and ED-adjacent settings. Its ExdionACE solution automates coding and revenue integrity using rule-based AI and ML, while ProMaxAI adds real-time analytics and AI-driven coding feedback to improve accuracy, speed, and compliance.
Key Features:
- ExdionACE auto-coding engine for ICD-10, CPT, E/M, and modifiers with built-in compliance checks
- ProMaxAI analytics with real-time dashboards and an AI chatbot (“Genie”) for coding guidance and denial prediction
- Revenue integrity and CDI with 100% chart review for missed charges and documentation gaps
- EMR-agnostic integration via APIs and bots with acuity and provider-level insights
- Real-time CAPD tools, compliance training, and automated claim submission
Best For: High-volume physician practices focused on E/M optimization, CDI, and faster TAT
10. Xpert Dox
XpertDox is an AI-powered autonomous medical coding platform focused on high-volume ambulatory and urgent care settings. Its XpertCoding solution automates the majority of coding with minimal human intervention, helping practices accelerate charge capture, reduce denials, and improve revenue cycle speed through EHR-integrated AI.
Key Features:
- Fully autonomous AI coding for ICD-10, CPT, HCPCS, E/M, and modifiers, covering >95% of claims
- Hybrid AI architecture using ensemble models, NLP, neural networks, and RPA
- BI dashboards for charge capture, CDI, denial analytics, audit trails, and provider performance
- EMR-agnostic integration with rapid charge submission and proactive charge recovery
- Performance-based coding support (Category II CPT) and MIPS quality tracking
Best For: Urgent care centers, primary care practices, and FQHCs with high encounter volumes
How to Compare ED AI Medical Coding Vendors
Before choosing a solution, it’s critical to know what actually separates an ED-ready platform from a generic automation tool. Here’s how to evaluate an AI medical coding solution for the emergency department:
1. Start with ED-specific use cases
Confirm whether the vendor supports both ED professional and facility coding, and whether it handles critical care, trauma, pediatric and psych ED, observation-in-ED, and high-acuity visits—not just low-complexity encounters.
Look for live ED deployments or case studies, not generic outpatient references.
2. Assess depth and safety of automation
Go beyond marketing claims.
Ask what percentage of ED charts can be safely auto-coded, broken down by visit type. Understand how the system expresses confidence, when charts are routed to human coders, and how ED accuracy is measured, audited, and validated.
3. Evaluate workflow fit and integration
Assess integration with EHRs (Epic, Cerner), encoders, groupers, and existing CAC tools. Understand when ED charts are coded (real-time vs. batch), how exceptions flow, and support for boarding, cross-midnight visits, and ED-to-observation scenarios.
4. Look at governance, QA, and rollout approach
Ask about ED-focused QA programs, dual-coding strategies, training for coders and clinicians, and phased rollouts—often starting with lower-risk ED visits before expanding to trauma and critical care.
Implementation Lessons from Real ED Deployments at CombineHealth
AI medical coding in the emergency department is hard for a few simple reasons:
- Care is overwhelmingly acute, not chronic
- E/M complexity depends on cognitive effort that’s often not explicitly documented
- Trauma rules, imaging interpretation, and chronic conditions influencing acute care must be captured
- Documentation is frequently incomplete or ambiguous due to ED time pressure
So when we implemented AI in ED coding workflows for this customer, we focused on one thing: teaching the system to reflect how experienced ED coders actually think.
Before assigning codes, our AI is designed to answer three questions:
- What actually happened during this encounter?
- What resources were used?
- What conditions or symptoms justify those charges?
That logic shaped how our AI medical coding solution, Amy, operates in ED workflows.
How CombineHealth’s AI Medical Coding Solution Amy Operates in the ED
Amy reviews:
- Provider-authored notes
- Procedures performed
- Facility resources used
- Tests ordered and independently interpreted
Once billable services are identified, Amy builds the clinical story that justifies them.
She starts from first principles:
- What symptoms did the patient present with?
- What acute issues required intervention?
- Which chronic conditions increased complexity or risk?
Then comes a second pass:
Does every CPT code have a clear justification in the ICD-10 set?
Moreover, Amy knows ambiguity in ED and is designed not to guess. Take the following cases, for example:
- “Dark emesis” is mentioned, but “hematemesis” is never documented
- A procedure is described, but the rationale isn’t clear
- A condition is implied across notes but never stated
- Different providers document the same event differently
In these cases, Amy escalates the chart, mirroring how experienced coders protect compliance and revenue.
Ready to accelerate your ED RCM workflows? Book a demo with CombineHealth to see how Amy can help!
FAQs
How accurate is AI at coding complex ED cases compared with experienced human ED coders?
In structured, well-documented cases, AI can match or approach experienced ED coder accuracy. However, in high-acuity or ambiguous cases (e.g., evolving sepsis or trauma), performance depends heavily on documentation clarity. Most mature systems combine AI automation with human review for complex, high-risk encounters.
Which ED encounters are safe to auto‑code, and which should always be manually reviewed?
Lower-acuity, well-documented visits with clear diagnoses and straightforward procedures are generally safer for auto-coding. Complex trauma, critical care, multi-problem encounters, ambiguous documentation, or charts with conflicting inputs typically require manual review to protect compliance and revenue integrity.
Will AI replace ED medical coders?
AI is more likely to change the role than replace it. Routine charts can be automated, allowing coders to focus on complex cases, audits, denial prevention, and education. Most ED deployments use a human-in-the-loop model where coders oversee, validate, and manage edge cases.
How does AI avoid increasing clinician burden with extra clicks, queries, or alerts in an already hectic ED environment?
Well-designed systems work in the background—reading existing documentation rather than forcing structured data entry. They escalate only when documentation gaps materially affect coding. Poorly designed tools can add friction, so workflow fit and thoughtful implementation are critical.
What ED‑specific benchmarks can vendors show from live deployments?
Strong vendors should provide ED-specific metrics such as automation rate by acuity level, coding accuracy vs. human audit results, denial reduction rates, turnaround time improvements, and impact on DNFB. Ideally, these benchmarks are drawn from comparable ED volumes and payer environments.







